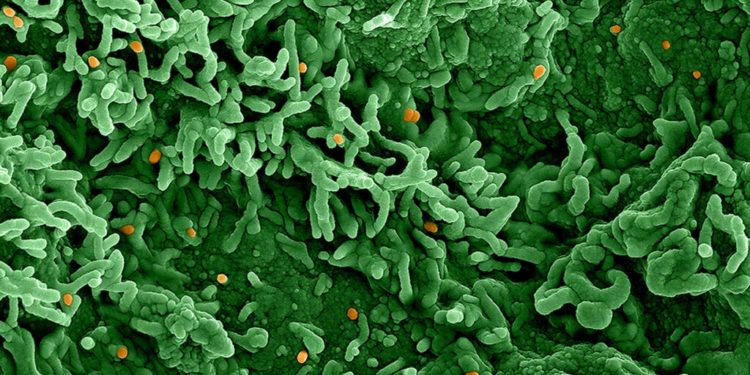
Just over three months in the past, public well being authorities within the U.Ok., Europe, and the U.S. started to sound the alarm on the arrival of monkeypox. Since then, this long-neglected tropical illness — which till this 12 months was largely restricted to periodic spillovers within the areas of Western and Central Africa the place the virus is endemic — has gone international. As of Aug. 26, 100 nations had reported almost 47,000 circumstances, in keeping with the World Health Organization.
The explosive epidemic has caught governments off-guard and despatched scientists scrambling to raised perceive the orthopoxvirus inflicting it.
In contrast to with SARS-CoV-2, they’re not ranging from scratch. Monkeypox shouldn’t be a brand new virus. It was first discovered in analysis monkeys at a lab in Denmark in 1958, and recognized as a human pathogen in 1970. However with little consideration from the worldwide group, monkeypox analysis acquired scant funding over the following a long time, leaving many key questions concerning the virus unanswered. The present outbreak, which is exclusive each within the pace of unfold and the methods during which individuals are changing into contaminated, has additionally prompted new ones.
commercial
STAT examined a number of the most urgent of those questions, lots of which received’t be resolved with out extra time and knowledge. Others could stay mysteries. However at the least in some circumstances, rising proof is starting to supply clues to what the eventual solutions could also be — clues which can be prone to form how public well being businesses and well being care techniques reply to the present outbreak, and the place it goes from right here.
The place does the rattling factor come from?
One factor we all know: Monkeys aren’t the unique supply of the monkeypox virus. What’s the precise reservoir host? That is a crucial however unanswered query.
commercial
A reservoir is a species that may carry a pathogen with out being sickened by it. Bats, as an example, are regarded as reservoirs for all types of nasty viruses — Marburg virus, its cousins, the assorted species of Ebola, and untold numbers of coronaviruses, amongst others. These viruses could be lethal in the event that they handle to make their means from bats to different species, together with our personal. However there’s no proof they hurt bats in any means.
As we’ve talked about already, monkeypox bought its title as a result of monkeys have been the primary species seen to be contaminated with this poxvirus. But it surely was seen as a result of the virus made the monkeys sick, that means they weren’t the reservoir.
Many species of animals can contract monkeypox. Hedgehogs, shrews, squirrels, anteaters, prairie canine — all these can contract the virus, and, underneath sure circumstances, transmit it to folks.
However all of the recognized rodents and different small mammals are victims of the virus, not the reservoir, Jean-Jacques Muyembe, the legendary microbiologist who runs the Nationwide Institute of Organic Analysis within the Democratic Republic of the Congo, cautioned throughout a current panel discussion hosted by the Harvard World Well being Institute.
The seek for the supply continues. That reality underscores an essential fact about monkeypox. Even when this multi-national outbreak is stopped, monkeypox will stay a menace.
(A fast P.S.: The speedy geographic unfold of monkeypox has sparked fears that the virus will get seeded into inclined species in components of the world the place it hasn’t historically been discovered, enlarging the world during which it’s endemic.
The Facilities for Illness Management and Prevention and different well being authorities have warned individuals who contract monkeypox to chorus from contact with any pets they could have, for that very motive. And a not too long ago published letter in The Lancet revealed the knowledge of that recommendation. A canine owned by two homosexual males in Paris seems to have contracted monkeypox from them.)
Why are lesions localized in some individuals who contract monkeypox, and disseminated in others?
Some individuals who contract monkeypox develop lesions over quite a lot of physique components — the torso, the face, the soles of toes, the palms of fingers, and particularly on this outbreak, which is going on largely in homosexual and bisexual males who’ve intercourse with males, within the anogenital space.
A number of the males contaminated on this outbreak have had their lesions located virtually solely on their penises or in or round their anuses.
Some, perplexingly, have had just a few lesions. Some identified circumstances have had a single lesion.
Why this puzzling vary of manifestations of lesions? That is one thing science doesn’t presently have a solution for, mentioned Anne Rimoin, a monkeypox professional on the College of California, Los Angeles. “It may very well be the dose,” she mentioned, referring to the quantity of virus an individual is uncovered to when contracting monkeypox. In different phrases, it might be a matter of whether or not publicity was the results of fleeting contact with lesions or a extra protracted occasion. Different elements could embrace the route of publicity — skin-to-skin or inhaled droplets, as an example. The immune standing of the individual being contaminated may additionally affect this consequence. “But it surely’s in all probability a mix of those parts,” Rimoin mentioned.
What position are asymptomatic people taking part in in transmission?
Monkeypox prefers to duplicate within the pores and skin and mucous membranes. That’s why scientists have a tendency to search out the best concentrations of virus within the lesions of contaminated people. It’s additionally why it could be stunning if folks with out such lesions have been spreading monkeypox to others.
However a number of small research have begun to lift issues about that chance.
Throughout a retrospective screening of anorectal swabs collected from greater than 200 asymptomatic males at a sexual well being clinic in Paris, French researchers found virus on 13 samples. One of many males later developed an anal rash and the opposite skilled sore throat and fever. Not one of the others ever reported signs. A similar study, not but peer-reviewed, from researchers in Belgium discovered three constructive samples out of 224 asymptomatic people.
But it surely’s nonetheless not clear whether or not folks with out signs can cross monkeypox on to others. If they’ll, then post-exposure ring vaccination methods won’t be adequate to include additional unfold of the virus. (Ring vaccination includes immunizing people who’ve been uncovered to monkeypox by shut contact with an contaminated individual. The thought is to catch folks early sufficient that their immune techniques can nip a possible an infection within the bud earlier than they grow to be contagious.)
Getting a greater grip on the extent of asymptomatic unfold would require way more testing, together with at-home, self-administered assessments, mentioned Celine Gounder, an infectious illness epidemiologist and editor-at-large for public well being at Kaiser Well being Information.
“We have to begin getting assessments in folks’s fingers and making it doable for any individual to swab themselves,” Gounder mentioned. “That might actually assist us get extra knowledge on this query.”
Can monkeypox, like Ebola, pose a post-infection danger of transmission?
Monkeypox is a poxvirus, as its title implies. Ebola is a filovirus. These are totally different beasts.
And but a quirk of Ebola viruses — and their shut cousin, Marburg virus — is casting a shadow over the present monkeypox outbreak.
Filoviruses can squirrel themselves away in components of the physique the place immune system weaponry can’t attain them. These are often called “privileged websites” — the eyeball, synovial fluid (the fluid in joints), spinal fluid, and most significantly for this dialogue, the testicles.
From the very earliest days of recorded outbreaks of filoviruses, there was a suspicion that survivors may harbor viruses and cross them to others, primarily by intercourse. Later, it grew to become clear that viral persistence, as it’s referred to as, is a characteristic of those infections. A portion of people that survive filovirus infections will undergo a relapse later; a Scottish nurse contaminated when she labored on the West African Ebola outbreak in 2014 had two subsequent resurgences of sickness. In different circumstances, male survivors have contaminated intercourse companions months, even years after recovering.
It isn’t recognized if monkeypox virus can equally lodge in testicles and pose a post-infection transmission danger. However the truth that scientists are discovering monkeypox viral DNA in semen, and in one case even managing to develop stay virus from semen, is elevating the query.
It’s thought that monkeypox is a one-and-done an infection, that individuals who survive — as most individuals do — have life-long immunity. They can’t be reinfected and pose no transmission danger after they recuperate. However that calculus modifications if survivors have monkeypox virus hiding of their testicles or different components of their our bodies.
Due to the unanswered questions, the Well being Safety Company in the UK is recommending males who’ve had monkeypox put on condoms throughout intercourse for at the least 12 weeks after recovering. The CDC says sporting condoms is advisable, however at current there is little data on which to make such a advice.
Do individuals who have recovered from monkeypox pose a near-term or longer-term transmission danger? It’s an essential query that must be answered. With such a big pool of monkeypox survivors to review, this outbreak ought to present alternatives to take action.
How properly does the vaccine work at lowering signs and stopping infections?
Each the CDC and the WHO estimate that the out there smallpox vaccines are about 85% efficient in opposition to monkeypox. However consultants warning that the extremely cited determine shouldn’t be taken at face worth, significantly within the context of the present outbreak.
The determine dates again to an observational study involving 245 folks contaminated with monkeypox in Zaire (now the Democratic Republic of the Congo) between 1981 and 1986, and greater than 2,000 of their contacts. People who had a visual scar from a jab with the first-generation smallpox vaccine have been about seven instances much less prone to contract monkeypox after publicity to an contaminated individual than those that have been unvaccinated.
Another study, additionally performed in Zaire within the Nineteen Eighties by the identical WHO monkeypox surveillance crew, took a better have a look at how the vaccine impacted the severity of signs. Amongst 282 sufferers — the overwhelming majority of them youngsters underneath the age of 15 — unvaccinated people have been twice as prone to have massive numbers of lesions crop up, and 3 times as prone to have a number of lesions within the genital space.
With out a smallpox shot, monkeypox sufferers typically suffered grotesque outcomes, together with problems that might flip lethal. The researchers reported that one out of 10 unvaccinated monkeypox sufferers died, with even increased fatality charges among the many youngest youngsters. One 5-year-old boy endured greater than 4,500 lesions earlier than succumbing to blood poisoning brought on by a secondary bacterial an infection. In distinction, not one of the vaccinated sufferers died.
The historic smallpox vaccines administered in these research are now not in manufacturing. However newer ones, like MVA-BN, a third-generation smallpox vaccine manufactured by Bavarian Nordic, are anticipated to have comparable efficacy in opposition to monkeypox, based mostly on studies in people that confirmed comparable antibody responses. Nonetheless, they haven’t been straight examined in opposition to the illness in medical trials.
MBA-BN, recognized within the U.S. as Jynneos, is presently the one vaccine on this nation licensed by the Meals and Drug Administration to forestall monkeypox an infection. Its preliminary approval for smallpox was based mostly on favorable knowledge from almost two dozen medical trials with greater than 7,500 contributors. However when the company later permitted the vaccine for monkeypox, its resolution was based on data from animal experiments, together with non-human primate research. Eighty to 100% of the monkeys who bought the jab later survived a deadly dose of the virus, in comparison with zero to 40% of the placebo group.
“I’m not conscious of any good knowledge on vaccine safety,” mentioned Rimoin. Surveillance studies performed by her group within the 2000s discovered hints that first-generation photographs had been efficient; 30 years after mass smallpox vaccination campaigns ceased in central Africa, incidence of monkeypox circumstances there elevated 20-fold.
However she doubts that such knowledge could be extrapolated to the present outbreak — which is primarily spreading by sexual contact. Mucosal surfaces are simpler for the virus to contaminate, and the extended contact that occurs throughout intercourse is probably going exposing folks to a lot bigger doses of the virus than the teams of people that have been studied in western and central Africa in earlier a long time.
“That is the crux of the issue,” mentioned Rimoin. “I believe that we predict extra from these vaccines than they have been designed for. This type of intense, usually repeat, mucosal exposures are very totally different from animal publicity, family, fomite, or respiratory droplet transmission.”
These maybe outdated estimates of vaccine effectiveness are based mostly on research of pre-exposure vaccination. There’s even much less knowledge supporting the ring vaccination technique being deployed by nations together with the U.S., the U.Ok., and Canada. That technique hinges on having rigorous contact tracing and a protracted incubation interval during which to function. And whereas the method has confirmed very efficient at curbing smallpox it’s not apparent but that it’s going to work as properly for monkeypox.
Up to now, there’s been only a single observational examine wanting on the query straight. In a paper launched (however not but peer-reviewed) earlier this month, researchers in France reported that amongst 276 high-risk contacts who have been vaccinated post-exposure, 12 of them later contracted the illness. Nonetheless it’s exhausting to say whether or not these have been true breakthrough infections as a result of most of them acquired their photographs greater than per week after the publicity, exterior the beneficial four-day window.
“It’s doable they developed the illness as a result of they have been vaccinated a bit too late,” mentioned Michaël Thy, a tropical infectious illness physician at Paris Cité College who led the examine. However he famous that not one of the 12 who skilled signs required hospitalization, indicating that post-exposure vaccination could scale back the severity of an infection, if not an infection itself.
The examine was small, and all of the contributors acquired a single dose of Jynneos so there’s no method to say whether or not the vaccine reduce the danger of an infection. The one means to do this is a randomized managed trial — with some folks getting the true deal and a few folks receiving a placebo shot.
Rimoin is among the many researchers racing to arrange such a examine. If the funding comes by, her group hopes to rapidly roll out trial websites in Los Angeles and the Democratic Republic of the Congo.
Till there’s extra knowledge, crucial factor that sufferers ought to know is that the vaccine, even two doses, doesn’t present 100% safety, mentioned Thy. “It’s an essential a part of a mixed technique for reducing the danger of an infection, nevertheless it’s not the one factor folks ought to be doing.”
Will the virus proceed to primarily infect males who’ve intercourse with males?
Within the U.S. and Europe, monkeypox has to date primarily affected males who’ve intercourse with males. However traditionally, outbreaks that start in a single group don’t stay there.
HIV famously unfold far past homosexual and bisexual males within the ’80s, fueled partly by officers who ignored early warnings that there was no such factor as a homosexual illness. Within the 2000s, an outbreak of drug-resistant micro organism was first noticed in homosexual males however finally unfold to athletes and took its best toll on folks in jail.
For now, monkeypox’s subsequent transfer stays unclear. A lot of the information is constructive: The virus seems to be harder to transmit by informal contact than initially feared, narrowing its potential paths. Circumstances have additionally been declining in New York, San Francisco, and far of Europe, as extra vaccines grow to be out there and folks reduce their danger of publicity by intercourse.
“There are some encouraging developments,” mentioned Chris Beyrer, an epidemiologist and incoming director of the Duke World Well being Institute. “If we will include this epidemic of this outbreak in males who’ve intercourse with males, that’s our greatest shot.”
And but the information shouldn’t be good in every single place. The monkeypox response has to date been marked by inequities. In North Carolina, 72% of individuals identified with monkeypox are Black, in keeping with knowledge launched earlier this month, however solely 24% of vaccines have gone to Black residents — a obtrusive instance of a racial disparity seen in much of the country.
The longer these disparities go unaddressed, the extra possible the virus is to stay round and unfold broadly, together with into prisons and different overcrowded settings, or to even grow to be endemic amongst animals in North America.
“We now have this window of alternative proper now. We now have encouraging knowledge that vaccination and habits change together are getting management of the outbreak in New York Metropolis,” mentioned Beyrer. “ I want the remainder of the nation regarded like New York proper now.”
When folks with monkeypox die, what do they die from?
One factor that’s changing into clear on this multi-country outbreak is that the monkeypox case fatality charge shouldn’t be as excessive as was beforehand estimated, at the least for clade II viruses (the previous West African clade) and when infections are primarily in adults. Figures starting from 1% to three% have traditionally been cited. However out of the almost 47,000 circumstances which have been detected to date this 12 months, there have been roughly 15 deaths reported.
A number of the questions we’re exploring right here aren’t presently answerable. For this one, there are knowledge — although not sufficient. Within the endemic nations, the place a lot of the monkeypox deaths have occurred, there haven’t at all times been detailed information of the causes of dying. However in case you dig into the scientific literature, there are some clues.
In 1987, researchers from the WHO’s long-defunct smallpox eradication unit and the Democratic Republic of the Congo’s monkeypox surveillance crew printed a major piece of work that charted the illness course of 282 individuals who contracted the virus between 1980 and 1985. (We referred to this examine within the part above on vaccine efficacy.) Within the paper, they in contrast severity of signs and outcomes of sufferers who had beforehand been vaccinated in opposition to smallpox — a vaccine in opposition to a associated virus that ought to supply some cross-protection in opposition to monkeypox — and people who had not.
There have been no deaths among the many monkeypox sufferers who had a smallpox vaccination scar. However among the many 250 who didn’t, there have been 27 deadly circumstances. All of the deaths occurred in youngsters underneath the age of 8, and the case fatality charge was greater than twice as excessive amongst these 4 years of age and youthful than amongst youngsters 5 to 9.
Nineteen of the youngsters who died developed bronchopneumonia and pulmonary misery. One developed septicemia, an an infection on the blood stream. One developed encephalitis — irritation of the mind.
A paper on Nigeria’s 2017-2018 monkeypox, printed within the journal The Lancet Infectious Ailments in 2019, reported that amongst 122 circumstances there, seven had been deadly. 4 of these have been individuals who have been dwelling with HIV however in whom the illness was untreated on the time of their monkeypox an infection. They died quickly, the authors reported, although they famous a exact reason behind dying was not out there in these circumstances.
Two different deaths have been attributed to secondary bacterial infections of monkeypox lesions, with obvious sepsis — a harmful situation the place the physique’s try and curb an an infection backfires and results in organ injury. The seventh dying was in a one-month-old toddler.
A systematic review printed in February in PLOS Uncared for Tropical Ailments — presciently titled “The altering epidemiology of human monkeypox — A possible menace?” — famous that from the Nineteen Seventies by the Nineteen Nineties, 100% of recorded deadly monkeypox circumstances have been in youngsters youthful than age 10. However within the first twenty years of this century, pediatric deaths declined to 37.5% of monkeypox circumstances.
And on this outbreak? What have the deadly circumstances died from?
Not less than a few these sufferers have been youthful males — one 31, one 44 — who weren’t immunocompromised and had no underlying continual ailments. These occurred in Spain. The boys each developed encephalitis.
A number of the deaths have occurred in immunocompromised folks. Late final month Brazil recorded a dying in a person who had lymphoma; Mexico not too long ago registered a dying in a person who was dwelling with HIV. He died from septic shock and pneumonia; his dying has not but been acknowledged as a monkeypox-related dying by the WHO. The post-mortem of an Italian vacationer who died not too long ago in Cuba reportedly revealed he had sepsis linked to pneumonia and organ injury. A dying in Ecuador was attributed to an unspecified pre-existing illness.
For a lot of the monkeypox deaths which have occurred this 12 months, nevertheless, there isn’t a exact reason behind dying that has made its means into the general public area. In at the least a few of these circumstances, scientific papers are in all probability already within the works. So we’ll must bide our time to get extra solutions.
Does having been vaccinated in opposition to smallpox a long time in the past defend in opposition to monkeypox in the present day?
The age distribution of circumstances exhibits there are far fewer infections amongst folks 60 and older — in different phrases, individuals who would have been vaccinated in opposition to smallpox once they have been youngsters. However is that the impact of safety from earlier vaccination or decrease charges of publicity in older males? Or each?
It’s not 100% clear. However it’s doable it has extra to do with danger of publicity than residual safety from a jab given a long time earlier.
The median age of circumstances within the international outbreak is 36. Males aged 18 to 44 make up 78% of all circumstances, in keeping with WHO knowledge. They’d be too younger to have been vaccinated in opposition to smallpox once they have been youngsters.
It’s obvious from a number of the research we cite on this article (see the references to the examine of 282 monkeypox circumstances in Zaire) that even again within the Nineteen Eighties, individuals who had been comparatively not too long ago vaccinated in opposition to smallpox may contract monkeypox. However they’d a milder course of sickness once they did.
A study performed in the USA after a rare monkeypox outbreak in 2003 sheds somewhat gentle right here. In that occasion, the primary recorded monkeypox outbreak exterior of Africa, three of the 47 individuals who contracted the virus have been utterly asymptomatic. That they had been vaccinated in opposition to smallpox once they have been younger — 13, 29, and 48 years earlier. 5 different folks beforehand vaccinated in opposition to smallpox developed monkeypox illness in that outbreak, however they’d, in the principle, fewer lesions than unvaccinated folks.
How lengthy does safety from prior smallpox vaccination final? Researchers have estimated that safety in opposition to extreme illness erodes after about 32 years and safety in opposition to deadly illness lasts almost 52 years. However these estimates are based mostly 1) on safety in opposition to smallpox (monkeypox safety from smallpox vaccine begins out already lowered) and a pair of) calculated utilizing knowledge from a 1903 smallpox outbreak in Australia.
Has the virus modified in any consequential means — or will it?
When scientists began sequencing the viruses behind this outbreak, what was notable was simply what number of mutations the pathogen had picked up in just a few years — and what clues these mutations contained. There was a priority early on that modifications to the virus’s genome had made it extra transmissible, explaining the unprecedented international unfold of the virus. Surely, although, the analysis has indicated that the mutations have been proof of a years-long combat with human immune techniques, not indicators of a basic change within the virus. These genetic scars left over from previous battles with immune techniques additionally offered a roadmap for scientists, who used them to estimate that this line of viruses has been spreading amongst folks since perhaps 2016.
Nonetheless, scientists try to find out if any of the mutations have given the virus some kind of benefit over different types of the virus, even when at this level there aren’t any apparent indicators they did. However one factor they do know is that, because the virus spreads extra, it has ever extra possibilities to maintain evolving and to maybe decide up mutations that might make it much more of a menace.
What occurs if particular person communities include their outbreaks?
There was a bit of fine information final week: The WHO reported that circumstances globally had declined 21% from per week prior, largely because of a drop in newly confirmed circumstances from Europe. Even domestically, as we famous above, documented circumstances are on the decline in New York and San Francisco, as public well being officers level to the affect of vaccination campaigns and behavioral modifications amongst these most in danger, together with lowering the variety of intercourse companions folks have.
Even when particular person cities, or nations, can get rid of monkeypox, they received’t be capable to transfer on totally. They’ll must proceed surveillance to make sure the virus didn’t get established in animals regionally — a supply for potential future outbreaks. And with the virus nonetheless spreading elsewhere — the WHO has famous that infections are nonetheless growing in Africa and Latin America — they’ll must be looking out for reintroductions, significantly as folks calm down a number of the behavioral modifications they’ve made.
But when outbreaks are actually introduced underneath management in locations in North America and Europe, the stress on these nations to handle the worldwide downside of monkeypox will solely enhance. Because the outbreak has proven, viruses which can be outlined as endemic to sure components of the world don’t simply keep there. Rich nations have additionally been criticized for not doing extra to assist the African nations which have animal reservoirs of the virus combat the pathogen, whilst there have been indicators of extra human-to-human transmission lately. Even now, as nations in Europe and North America have scooped up international vaccine provides, these African nations don’t have entry to vaccines. On the earth of infectious ailments, reminiscence is usually quick, and the general public can rapidly transfer on when one thing is now not deemed a menace to them. We’ll see if this time is totally different.